Living with diabetes comes with its challenges, and one lesser-known but critical aspect is its impact on vision. Diabetes can lead to various eye complications, ultimately resulting in vision loss if not managed effectively. In this article, we’ll delve into seven essential facts about vision loss due to diabetes, offering insights, tips, and strategies to safeguard your eye health.

7 Facts About Vision Loss Due to Diabetes
Understanding Diabetic Retinopathy: The Primary Concern
Diabetic retinopathy stands as the leading cause of vision loss among individuals with diabetes. This condition affects the blood vessels in the retina, leading to damage and potential vision impairment.
Diabetic retinopathy progresses through stages, starting with mild non-proliferative retinopathy to severe proliferative retinopathy. Regular eye exams are crucial for early detection and intervention.
The Impact of Diabetic Macular Edema (DME)
Diabetic macular edema, a complication of diabetic retinopathy, occurs when fluid accumulates in the macula, the central part of the retina responsible for sharp vision. DME can cause blurry vision and, if left untreated, may lead to permanent vision loss.
Early diagnosis and timely treatment, such as laser therapy or anti-VEGF injections, can help manage DME effectively and preserve vision.
Glaucoma and Diabetes: Understanding the Connection
People with diabetes have an increased risk of developing glaucoma, a group of eye conditions characterized by damage to the optic nerve. Elevated intraocular pressure, common in diabetes, contributes to this heightened risk.
Regular eye screenings and early detection are essential for managing glaucoma effectively and preventing irreversible vision loss.
Cataracts: Another Challenge for Diabetics
Cataracts, a clouding of the eye’s lens, are more prevalent and tend to progress faster in individuals with diabetes. Poorly managed blood sugar levels accelerate cataract formation, leading to compromised vision.
Maintaining optimal blood glucose levels and undergoing timely cataract surgery, when necessary, can help restore clear vision and prevent further deterioration.
The Importance of Blood Sugar Control
Effective blood sugar management is paramount in preventing and mitigating diabetic eye complications. Consistently high blood glucose levels damage the small blood vessels in the retina, contributing to diabetic retinopathy and other eye issues.
By closely monitoring blood sugar levels, adhering to a balanced diet, exercising regularly, and following prescribed medications, individuals can significantly reduce their risk of vision loss.
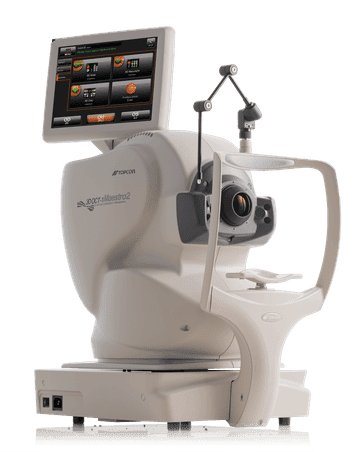
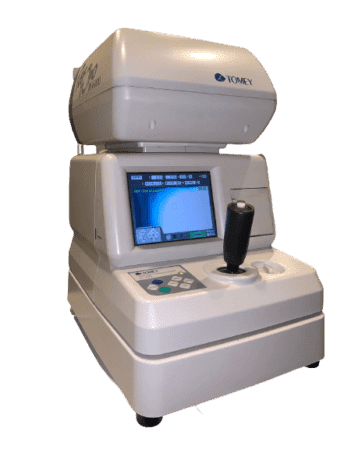
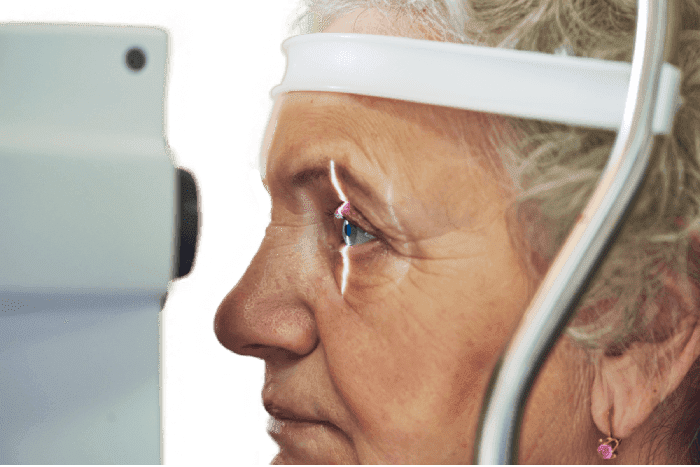
Regular Eye Exams: Key to Early Detection and Intervention
Routine eye examinations play a pivotal role in preserving vision for individuals with diabetes. These comprehensive exams enable eye care professionals to detect early signs of diabetic eye diseases, allowing for timely intervention and treatment.
Yearly dilated eye exams are recommended for individuals with diabetes, even in the absence of apparent vision problems.
Lifestyle Modifications for Eye Health
In addition to medical management, certain lifestyle modifications can help protect vision and minimize the risk of diabetic eye complications. These include:
- Maintaining a Healthy Diet: Emphasize a diet rich in fruits, vegetables, whole grains, and lean proteins while limiting processed foods and sugary snacks.
- Regular Exercise: Engage in regular physical activity to improve blood circulation and promote overall health.
- Smoking Cessation: Quitting smoking can significantly reduce the risk of diabetic eye diseases and other systemic complications.
- UV Protection: Wear sunglasses with UV protection to shield your eyes from harmful ultraviolet rays.
By incorporating these lifestyle changes, individuals can proactively safeguard their eye health and reduce the likelihood of vision loss associated with diabetes.
FAQs (Frequently Asked Questions)
- How does diabetes affect vision? Diabetes can cause various eye complications, including diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma, ultimately leading to vision loss if left untreated.
- Are there any warning signs of diabetic eye complications? Yes, symptoms such as blurry vision, floaters, sudden vision changes, or difficulty seeing at night may indicate diabetic eye issues and warrant prompt evaluation by an eye care professional.
- Can diabetic eye complications be prevented? While diabetic eye diseases cannot always be prevented, proactive management of blood sugar levels, regular eye exams, and lifestyle modifications can significantly reduce the risk and severity of complications.
- How often should individuals with diabetes undergo eye exams? Yearly dilated eye exams are recommended for individuals with diabetes, regardless of whether they experience vision problems, to detect early signs of eye disease and prevent vision loss.
- What treatment options are available for diabetic eye complications? Treatment options may include medications, laser therapy, intraocular injections, or surgical interventions, depending on the specific condition and its severity.
- Is vision loss reversible in diabetic eye diseases? Early detection and timely intervention can often prevent further vision loss and may even restore some degree of lost vision. However, advanced cases of diabetic eye disease may result in permanent vision impairment.
Conclusion
In conclusion, understanding the relationship between diabetes and vision loss is crucial for effectively managing eye health. By staying informed, proactive, and vigilant, individuals can minimize the risk of diabetic eye complications and preserve their precious eyesight for years to come.
Tatum Eyecare is North Phoenix’s premier family eye care center. We’ve spared no expense to create the most pleasant, comfortable patient experience… including the finest furnishings, the best selection of prescription eyeglass frames, the most cutting-edge technology, and the most outstanding team of industry professionals. Come see why the choice for family eye care in the Valley has never been clearer.




































 Dillon Optics, the performance eyewear arm of Dillon Precision, have a unique non-reflective, matte lens appearance incorporated with NIR lens technology. This produces noticeably sharper clarity, and protects the lens from damage and harmful environmental conditions. Perfect for outdoor sports and activities where precision vision is required. Tatum Eyecare carries a wide variety of Dillon Optics eyewear.
Dillon Optics, the performance eyewear arm of Dillon Precision, have a unique non-reflective, matte lens appearance incorporated with NIR lens technology. This produces noticeably sharper clarity, and protects the lens from damage and harmful environmental conditions. Perfect for outdoor sports and activities where precision vision is required. Tatum Eyecare carries a wide variety of Dillon Optics eyewear.